Dual diagnosis cases present unique challenges in addiction recovery. At Ona Treatment Center, we understand the complexities of managing co-occurring mental health and substance use disorders.
Effective dual diagnosis relapse prevention requires a comprehensive approach that addresses both conditions simultaneously. This blog post explores strategies to help individuals with dual diagnoses maintain long-term recovery and improve their overall well-being.
What Is Dual Diagnosis?
Definition and Prevalence
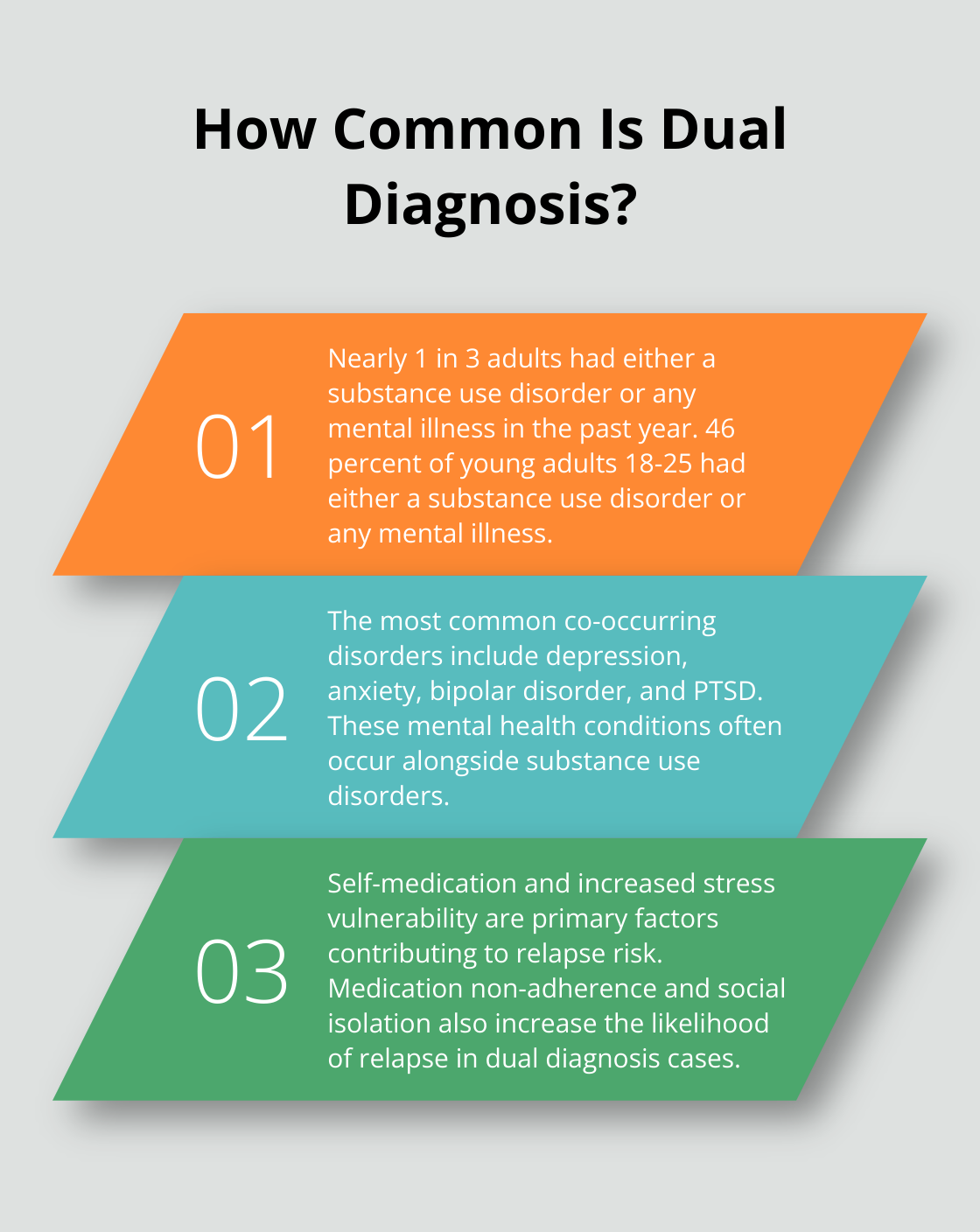
Dual diagnosis, also known as co-occurring disorders, refers to the simultaneous presence of a mental health disorder and a substance use disorder in an individual. This complex condition affects a significant portion of those seeking treatment for addiction or mental health issues. Nearly 1 in 3 adults had either a substance use disorder or any mental illness in the past year, and 46 percent of young adults 18-25 had either a substance use disorder or any mental illness.
Common Co-occurring Disorders
The most frequently observed co-occurring disorders include:
-
Depression
-
Anxiety
-
Bipolar disorder
-
Post-traumatic stress disorder (PTSD)
These mental health conditions often occur alongside substance use disorders.
Factors Increasing Relapse Risk
Several factors contribute to the heightened relapse risk in dual diagnosis cases:
Self-Medication
Self-medication is a primary concern, where individuals use substances to alleviate symptoms of their mental health condition. This behavior can lead to a vicious cycle, as substance use often worsens mental health symptoms in the long run.
Stress Vulnerability
People with dual diagnosis often show increased susceptibility to stress, which can trigger both mental health symptoms and substance cravings. A study published in the Journal of Substance Abuse Treatment found that stress management skills play a vital role in preventing relapse.
Medication Non-Adherence
Some individuals may stop taking prescribed psychiatric medications due to side effects or a false sense of improvement. This can lead to a resurgence of mental health symptoms and potential substance use.
Social Isolation
Social isolation, common among those with dual diagnosis, can further increase relapse risk. A study in the Journal of Substance Abuse Treatment highlighted that individuals with strong support networks (family, friends, and support groups) have better recovery outcomes.
Understanding these risk factors forms the foundation for developing effective relapse prevention strategies. A comprehensive assessment to identify each patient’s unique risk factors (including genetic predisposition and environmental triggers) allows for a tailored treatment approach. This personalized strategy sets the stage for creating a robust relapse prevention plan, which we will explore in the next section.
Creating Your Personalized Relapse Prevention Strategy
Identify Your Unique Triggers
The first step in creating your relapse prevention plan is to identify your specific triggers. These can include people, places, emotions, or situations that increase your risk of relapse. Common triggers include:
-
Stress at work or in relationships
-
Financial difficulties
-
Negative emotions (e.g., anger or sadness)
-
Certain social situations or peer pressure
-
Physical pain or discomfort
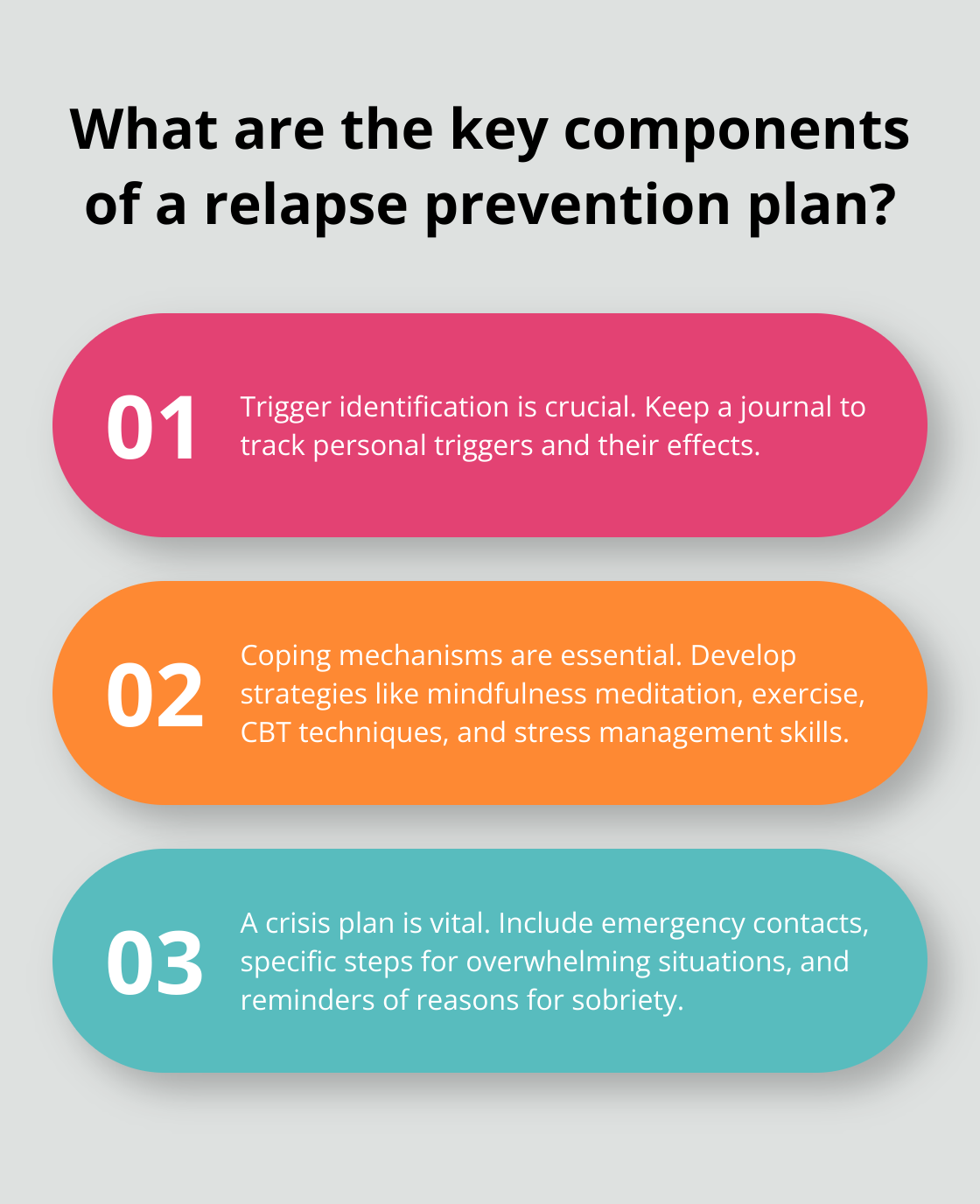
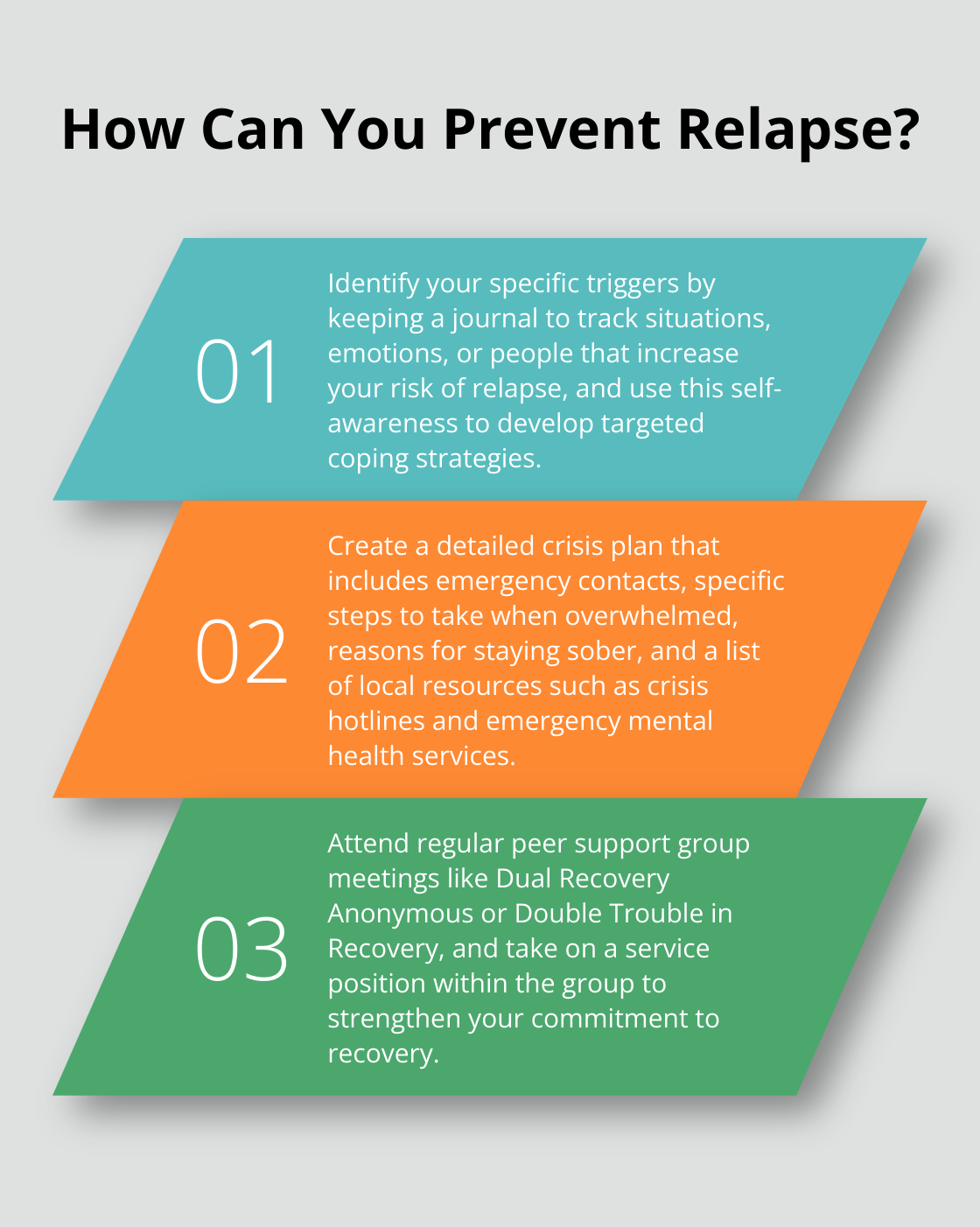
Keep a journal to track your triggers and their effects on you. This self-awareness will help you develop effective coping strategies.
Develop Coping Mechanisms
After you identify your triggers, develop healthy coping mechanisms. These should address both your mental health symptoms and substance use urges. Some effective strategies include:
-
Mindfulness meditation: This practice can improve emotion regulation and reduce drug abuse.
-
Exercise: Regular physical activity boosts mood, reduces stress, and decreases cravings. Try to engage in at least 30 minutes of moderate exercise most days of the week.
-
Cognitive Behavioral Therapy (CBT) techniques: Learn to challenge negative thought patterns and develop healthier ways of thinking.
-
Stress management skills: Practice deep breathing, progressive muscle relaxation, or yoga to manage stress effectively.
Create a Crisis Plan
Despite our best efforts, there may be times when relapse feels imminent. Having a crisis plan in place can make all the difference. Your plan should include:
-
A list of emergency contacts (including your therapist, sponsor, and supportive friends or family members)
-
Specific steps to take when you feel overwhelmed (such as calling a support person or attending a support group meeting)
-
Reminders of your reasons for staying sober and managing your mental health
-
A list of local resources (including crisis hotlines and emergency mental health services)
Review and update your relapse prevention plan regularly. As you progress in your recovery, your needs and challenges may change. Stay flexible and open to adjusting your strategies as needed.
Personalized Treatment Approaches
At Ona Treatment Center, we understand that no two individuals are alike, and their recovery plans shouldn’t be either. Our “Living in Balance” program provides support for family members of people with alcohol or drug abuse problems. We work closely with each client to develop and refine their personalized relapse prevention plan.
As we move forward, let’s explore the importance of building a strong support system in your recovery journey. This network of care will complement your personalized relapse prevention strategy and provide additional resources for maintaining your progress.
Building Your Recovery Network
Engage Family and Friends
Family and friends play a vital role in your recovery process. Supportive family relationships are associated with decreased risk of recurrence in substance use disorders.
To effectively involve your loved ones:
- Educate them about dual diagnosis and its challenges
- Communicate your needs and boundaries clearly
- Include them in your treatment plan, when appropriate
- Encourage their participation in family therapy sessions or support groups for families of individuals with dual diagnoses
Harness the Power of Peer Support
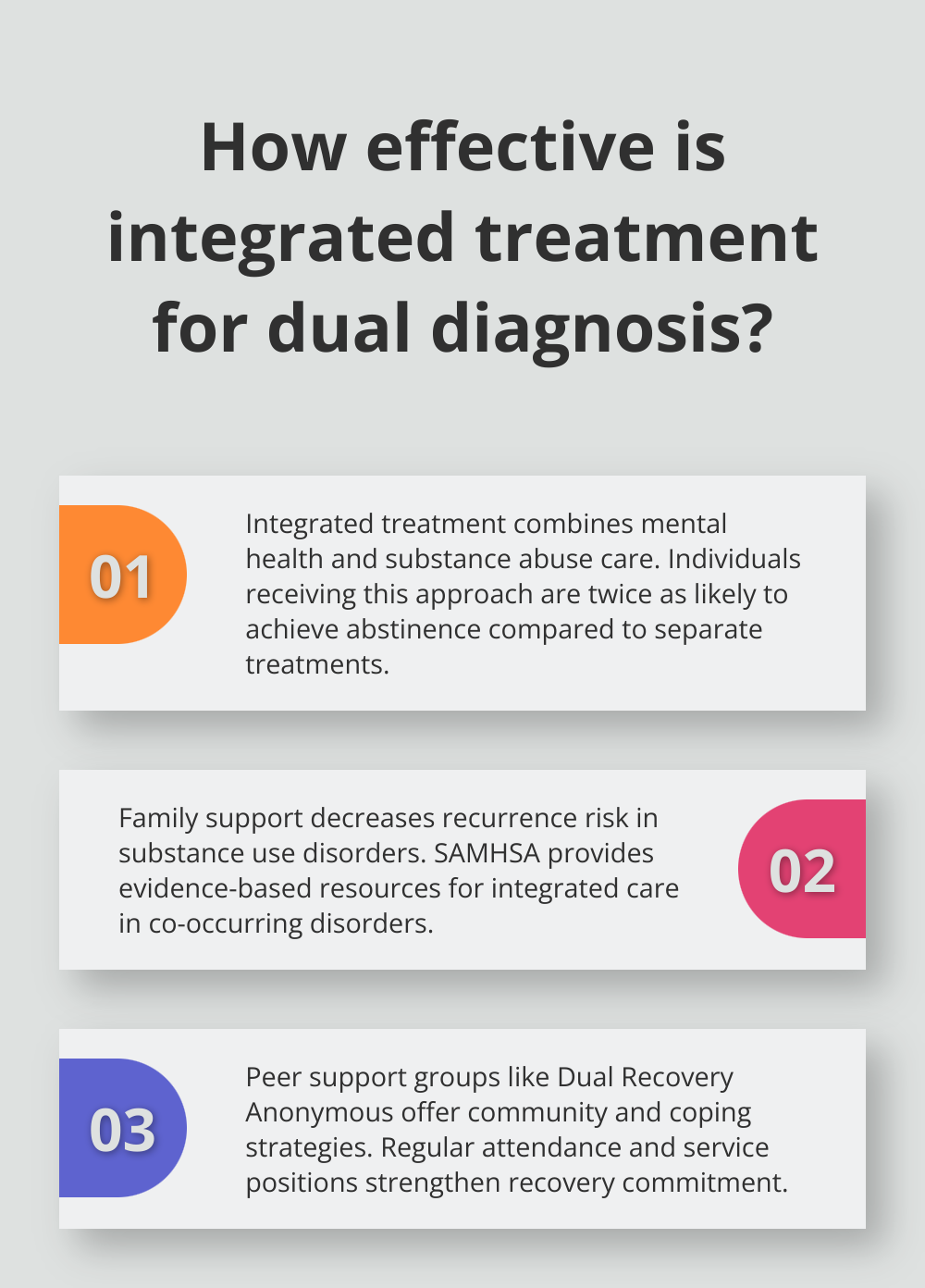
Peer support groups provide a sense of community, shared experiences, and practical coping strategies. SAMHSA offers evidence-based resources to help providers screen, diagnose, and deliver integrated care to patients with co-occurring disorders.
Consider joining groups such as:
- Dual Recovery Anonymous (DRA)
- Double Trouble in Recovery (DTR)
- SMART Recovery
Attend meetings regularly and take on a service position within the group to strengthen your commitment to recovery.
Leverage Professional Support
Professional support forms the backbone of your recovery network. This includes therapists, counselors, and sponsors who provide specialized guidance and accountability.
A study in the Journal of Clinical Psychiatry found that individuals with dual diagnoses who received integrated treatment from mental health and substance abuse professionals were twice as likely to achieve abstinence compared to those who received separate treatments.
To maximize the benefits of professional support:
- Keep regular appointments with your therapist and psychiatrist
- Be honest about your struggles and progress
- Work with your treatment team to adjust your recovery plan as needed
- Consider working with a sponsor from a 12-step program for additional support
Create a Comprehensive Support System
A robust support system acts as a safety net, providing emotional support, practical assistance, and accountability throughout your journey. This network should include a combination of family, friends, peers, and professionals.
Try to build relationships with individuals who understand and support your recovery goals. Attend support group meetings (both for mental health and substance use disorders) to expand your network and learn from others’ experiences.
Final Thoughts
Dual diagnosis relapse prevention requires a multifaceted approach that addresses mental health and substance use disorders simultaneously. Understanding your unique triggers, developing effective coping mechanisms, and creating a comprehensive crisis plan will lay the foundation for long-term recovery. A strong support network (including family, friends, peers, and professionals) contributes significantly to a robust recovery journey.
Relapse prevention for dual diagnosis is an ongoing process that demands continuous effort and commitment. Setbacks can happen, but they don’t define your recovery. Each day presents an opportunity to strengthen your resilience and refine your strategies.
At Ona Treatment Center, we understand the complexities of dual diagnosis and offer personalized, evidence-based treatment to support your recovery journey. Our “Living in Balance” program provides comprehensive care in a peaceful Northern California setting. If you’re struggling with co-occurring disorders, don’t hesitate to reach out to Ona Treatment Center.